Lupine Publishers | Open Access Journal of Oncology and Medicine
Multiple myeloma accounts for <1% of all malignancies and Central
nervous system (CNS) manifestation of multiple myeloma
(MM) is rare. Multiple myelomais characterized by malignant
transformation of plasma cells that produces immunoglobulin chains.
The accumulation of plasma cells in bone marrow results in clinical
features like anaemia, osteolytic lesions, hypocalcaemia, renal
failure and immunodeficiency [1,2]. The involvement of central nervous
system is very uncommon in multiple myeloma and it
may present early or late during the course of disease. The neurological
symptoms can be diffuse headache, persistent vomiting,
vertigo, weakness in limbs, urinary incontinence etc. Symptoms can be
attributed to spinal cord or nerve root compression,
peripheral neuropathies, and uremia [3,4]. Likely risk factors of CNS
manifestation are unfavourable cytogenetics, high tumour
load, low marrow involvement. In this report we describe a patient with
CNS involvement after receiving systemic chemotherapy
and symptomatic treatment.
Keywords: Central nervous system, Multiple myeloma
Case Report
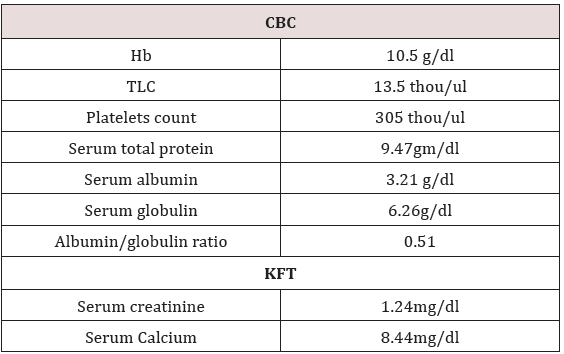
A 52 years pleasant lady presented with complaint of pain in
left leg with lower backache and tingling sensations for 10 days.
Subsequently she developed pain in right leg followed by urine
incontinence. MRI Lumbosacral Spine was done which reported
ill defined lesions at L3-L4 vertebra (with associated periosseous
fluid collections) and multiple focal lesions in the L4 vertebra,
bilateral sacral ala and both iliac bones along with indentations
upon the thecal sac by spondyliticridges, secondary spinal canal
stenosis and neural foraminal narrowing at multiple levels and
left exiting nerve root compression at L3-L4, L5-S1 levels (Table
1). She underwent L1-L5 stabilization, L3 decompression with
laminectomy, biopsy, posterolateral fusion with local autograft.
Histopathology reported plasma cell dyscrasia at L3-L4 level.
Immunohistochemistry reported tumor cells are focally positive for
CD-138 and kappa light chain and negative for lambda light chain.
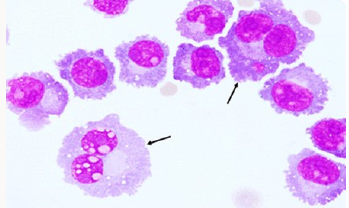
On further evaluation bone marrow biopsy reported plasma cells
approximately 50% of total nucleated cells suggestive of plasma
cell myeloma. Bone marrow aspiration shows plasmacytosis
approximately 24% of total nucleated cells which confirmed the
diagnosis. She received 15 cycles of Bortezomib and Thalidomide.
Table 1:
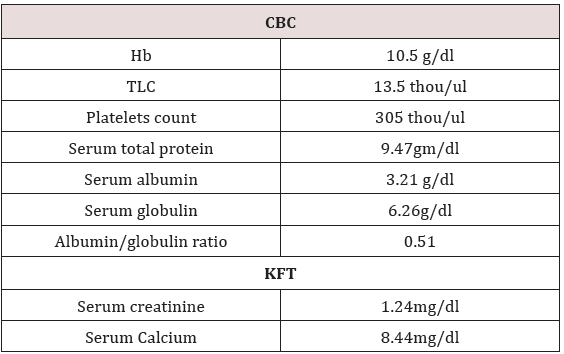
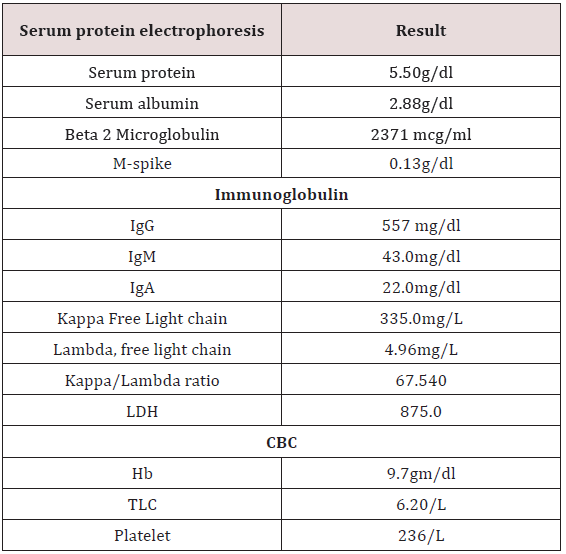
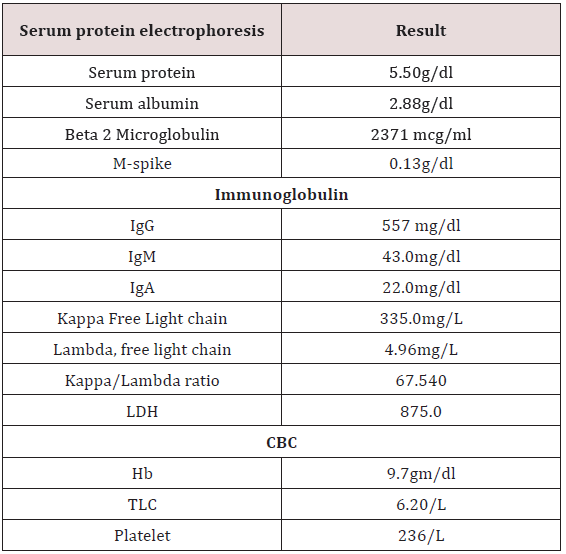
Table 2:
In view of persistent pain in legs MRI dorsal spine was done
which reported well defined altered intensity expansile lesion in
L3 vertebra extending into epidural space. She received palliative
external beam radiotherapy to L3 vertebra 30Gy/10 fractions. She
remained asymptomatic for a month. Then she presented with
complaint of lower limbs weakness and nausea, loss of appetite,
constipation, weight loss (Table 2). USG whole abdomen was done
which reported multiple hypoechoic masses in epigastric region.
Whole body PET CT reported metabolically active soft mass lesion
in gastro hepatic region measuring 9.7x5.5 cm SUV max 20.3, recto
uterine pouch measuring 9.2 x 7.8cm SUV 20.9, left iliac fossa
measuring 7.2x4.0cm- ?mitotic, metabolically active mesenteric
nodes measuring upto 2.2cm-? mitotic and metabolically active
lytic lesion involving L3 vertebra with paravertebral soft tissue
component infiltrating left psoas muscles.
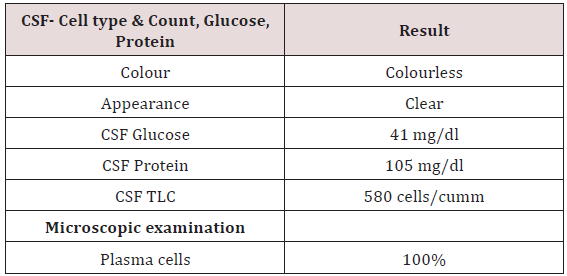
Table 3:
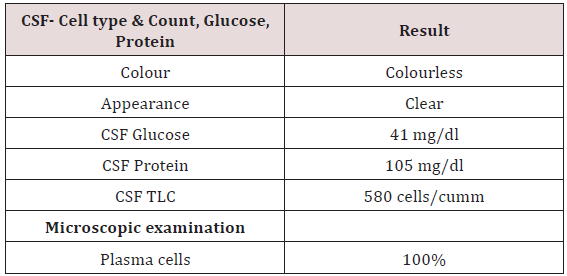
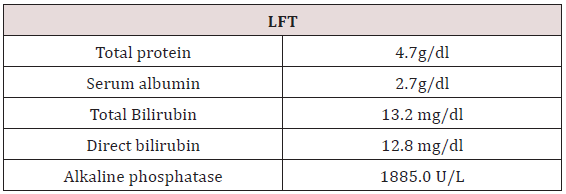
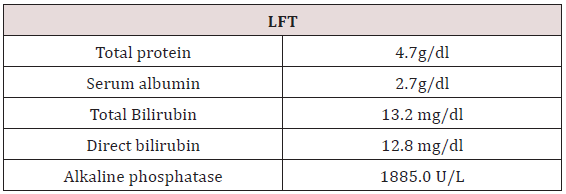
Table 4:
To confirm the diagnosis CT guided core needle biopsy from
supraumbilical mass was done which was compatible with
multiple myeloma. She then received 1st cycle of Bortezomib,
cyclophosphamide and dexamethasone. After few days, she
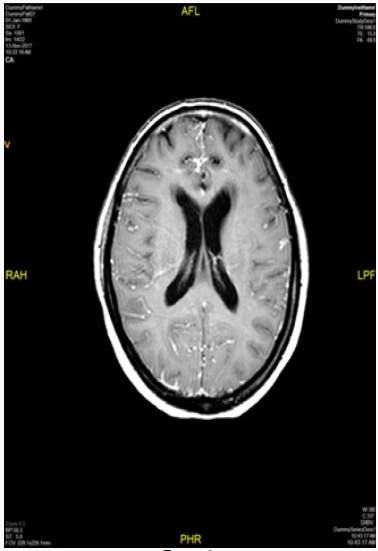
developed headache, giddiness and syncopal attacks. On evaluation
CEMRI brain reported diffuse leptomeningeal enhancement
involving both cerebral as well as cerebellar hemispheres. Mild
enhancement of basal cistern with associated marginal dilation
of ventricular system (Figure 1). In view of above mentioned
complaints, cerebrospinal fluid study was done (Table 3) (Figure 2).
CEMRI spine was done which reported no abnormal enhancement
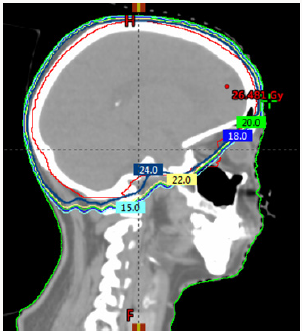
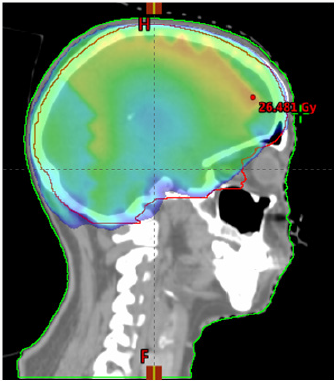
in vertebra, cord or thecal sac (Figures 3 & 4). She received 7
fractions (14 Gy) out of 12 planned fractions (24Gy) of whole brain
radiotherapy and two intra thecal injection of methotrexate. MRI
upper abdomen with MRCP reported large mass replacing entire
head and body region of pancreas. Mass encases and compresses
CBD with mild bilobar intra hepatic biliary radical dilation. There
is also encasement of second part of duodenum with possible
infiltrartion of adjacent hepatic parenchyma as well. Features are
suggestive of aggressive pancreatic malignanacy, possibility of
pancreatic lymphoma. Thickening and edema of gall bladder wall
was seen which was suggestive of concomitant cholecystitis. She
was advised for ERCP with SEMS placement which was refused by
attendants (Figure 5). In view of her deranged liver function test,
both radiotherapy and methotrexate were discontinued and she
was maintained on supportive care (Table 4).
Figure 1:
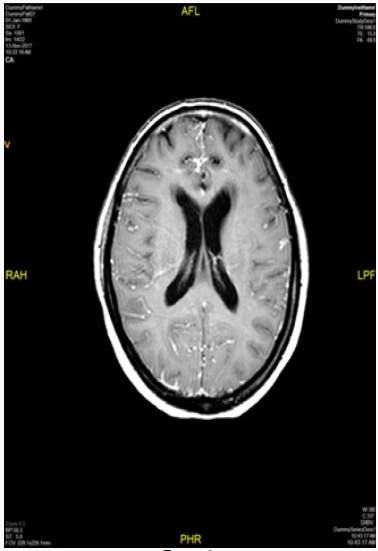
Figure 2:
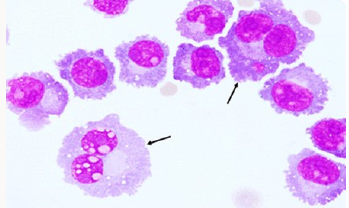
Figure 3:
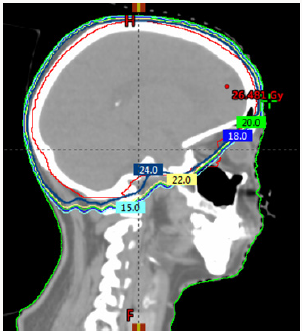
Figure 4:
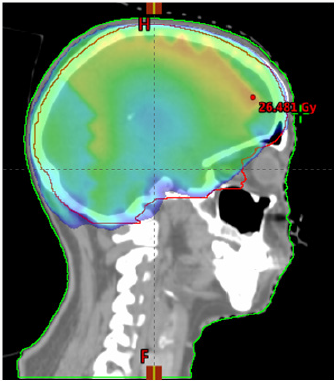
Figure 5:

Discussion
Central nervous system is a rare location of involvement
in MM, however it should be considered if a patient with MM
presents with neurologic symptoms. Patients with MM often have
neurological complications, either due to metabolic disorders such
as hypocalcaemia, uraemia and hyper viscosity or due to peripheral
neuropathy, spinal cord compression and cranial nerve infiltration
[1,2]. The most common cause is spinal cord compression and
cranial nerve infiltration [3,4]. The patient may present as a known
case of MM with CNS features or as a new case with CNS symptoms.
The clinical presentation depends on degree and site of infiltration.
The symptoms and signs are headache, memory loss, behavioural
changes, convulsions, nausea, vomiting, vertigo, urinary
incontinence, backache, and limb weakness [3,4]. These symptoms
can be attributed to spinal cord or nerve root compression, raised
intracranial tension, meningeal inflammation [5]. In our case
she presented with the complaint of headache, giddiness and
syncopal attacks. This can be explained by CEMRI brain imaging
which reported diffuse leptomeningeal enhancement involving
both cerebral as well as cerebellar hemispheres. CSF study was
done to reported to be negative. She received 7 fractions out of 12
fractions planned for whole brain radiotherapy and two injections
of intrathecal Methotrexate injections [6]. In view of deranged LFT,
radiotherapy and IT chemotherapy was stopped and was managed
conservatively. She passed away after 2 weeks due to sepsis with
LRTI with MM as underlying cause.
Conclusion
In conclusion this patient had an aggressive disease in view
of abdominal deposits and unresponsiveness to multiple lines of systemic disease. CNS involvement in cases of MM portends
extremely poor prognosis and median overall survival of <6
months. While in this case there was CSF infiltration which would
portend even poorer prognosis but she succumbed to sepsis due
to Lower respiratory tract infection. CNS disease in MM can be
effectively palliated especially because of relative radio sensitivity
of MM due to which early responses are seen at lesser doses and an
early diagnosis can improve quality of life effectively.
To Know More About Open Access Publishers Please Click on Lupine Publishers




No comments:
Post a Comment